
Spinal Decompression Therapy
Spinal Decompression Therapy
At our clinic we offer Non Surgical Spinal Decompression Therapy which is an alternative to surgery, and is non invasive and suitable for acute and chronic pain conditions in the neck and lower back regions of the spine.
Spinal Decompression Therapy is pain free and can provide relief from sciatica, arm and/or leg pain and numbness caused by slipped discs, bulging discs, disc herniation and degenerative disc disease.
By relieving the pressure from the discs and joints through gentle and specific stretching of the spine, therapy is aimed to reduce pain and increase mobility in a safe and comfortable procedure.
If you are considering surgery, contact us now to discuss whether Spinal Decompression Therapy is suitable for you!
- Non Invasive – therefore there is no risk of infection, scarring
- No recovery time – you can continue most of your normal daily activities
- All Natural – drug free
WHAT IS NON SURGICAL SPINAL DECOMPRESSION?
Spinal Decompression therapy is a revolutionary non-invasive treatment for low back, neck and nerve pain that radiates down the arms and legs. Not to be confused with traction, Spinal Decompression Therapy is successful in relieving pain associated with disc herniation/compression and Osteoarthritis. Decompression therapy may also provide a less invasive alternative for patients indicated for surgical intervention. Spinal decompression is suitable for:
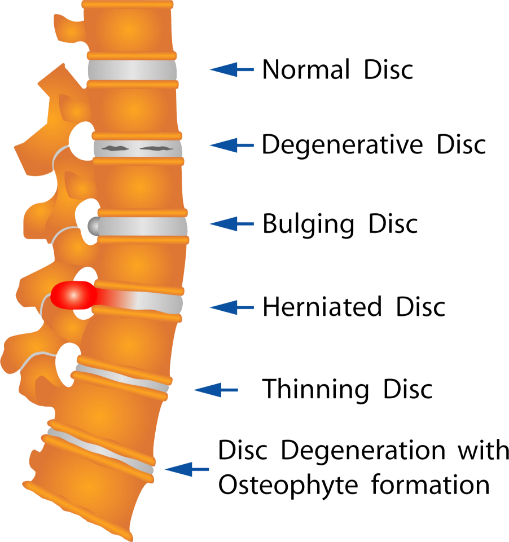
- Disc bulges/ herniations/ protrusions
- Sciatica/nerve pain
- Disc compression/Degeneration (DDD)
- Stenosis
- Post-surgical pain
- Lumbar/Cervical radiculopathies
- Osteoarthritis
- Arm/leg pain and numbness
- Chronic neck or back pain that is not responding to traditional spinal treatment.
Spinal Decompression Therapy is conducted on the revolutionary Hill DT Spinal Decompression Table, designed by Doctors of Chiropractic originating from the US. The Hill DT Spinal Decompression table is a specifically designed, computerised system which provides extremely gentle, precise and effective pulling forces to draw apart the vertebrae and release the pressure surrounding the targeted disc. This process also draws nutrients back into the disc leading to rehydration and healing.
Although relatively new in Australia, test case results from the US where this treatment has been available for several years have shown this treatment to be successful in 86% of cases.*
HOW DOES SPINAL DECOMPRESSION WORK?
When a bulging or herniated disc slips out of alignment, it may compress nearby nerves, causing pain and symptoms. It should be noted that as long as compression continues, damaged discs seldom heal on its own and patients will suffer pain and other symptoms.
 Compressed, bulging disc – pressing on the nerves
Compressed, bulging disc – pressing on the nerves
Spinal Decompression Therapy creates space between the different vertebrae, providing room for the bulging or herniated disc to be drawn back into its central position in the spine. This relieves pressure on the nerves and the surrounding soft tissues. By reversing the effects of axial load or compression in the spine, increased circulation occurs which facilitates the flow of nutrients, oxygen and fluids back into the disc which helps stimulate the body’s healing mechanism.
 Healthy, full height, hydrated disc – supporting the spine
Healthy, full height, hydrated disc – supporting the spine
REASONS TO CHOOSE SPINAL DECOMPRESSION
- To aid in the relief of chronic pain caused by bulging or herniated discs and degenerative disc disease
- An alternative to surgery or when surgery is not recommended
- When current treatments are not working
- To achieve a reduced need/dependency on painkillers
- To achieve long-term pain relief
- To enable a return to normal daily activities1
Spinal Decompression Therapy FAQ’s
All patients will require an initial assessment with our Chiropractor where you will be assessed for suitability.
You are required to bring your X-rays, CT or MRI scans on your first visit. Your initial consult would take about 40 minutes.
Our Chiropractor will take you through a detailed history of your health and complete a thorough examination (which would normally include chiropractic, orthopaedic and neurological examination). Upon completion of the spinal assessment our Chiropractor will advise you if you are a suitable candidate for Spinal Decompression Therapy. If you are ready to commence treatment, our Chiropractor will complete a program tailored for your condition.
You will be fully clothed and you will be required to lie down on the table where you will be securely fastened into a harness (either neck or lower back). The computerized program controls the table, slowly moving, lengthening and releasing the spine at precise intervals, decompressing the disc which would thereby take the pressure off the nerves.
Traction does not provide the special logarithmic movement, systematically increasing and decreasing the decompression the way that the Hill DT table does.
This cycle of movement is a critical part of the success of this therapy, as it brings the essential oxygen and nutrients to the area to help it heal.
A common side effect of traditional traction therapy is muscle splinting and guarding during treatment, impeding decompression. The Hill DT table does not allow your muscles to splint or guard as the seven sensors on the table are continually monitoring the muscles in the target area, maximizing decompression without side effects.
One of the most positive things about Spinal Decompression Therapy is how remarkably comfortable it is. Patients feel no pain and in most cases they find the treatment experience very relaxing.
You will feel intervals of gentle pulling then release for the 20 minutes that you are on the table, most people get used to it quite quickly and falls asleep for the treatment.
Only a small percentage of patients experience temporary soreness which is a sign that muscles have been stretched in a different way.
No. The treatment is non invasive – so there is no risk of infection; there is no recovery time – so there is no down time from daily activities; and it is all natural – as there are no drugs involved.
Some people do feel a change after just one or two sessions, others after about 5 -8 sessions, and others not until their 25th or 30th session. It all depends on how much inflammation you have, how long you have had the problem, how severe the problem is, and how well you follow our guidelines regarding nutrition, supplements and activities. Every case is different and we can give no guarantees regarding how long you may take to get better, nor if you will get better at all.
*All our patients are required to have 2-3 sessions of Spinal Decompression Therapy each week (minimum of 30 sessions altogether) for the treatment to be effective.
There are a few circumstances which may prevent you from being a candidate for decompression therapy.
Some of these reasons include if you weigh over 155kg, are pregnant (for lower back treatments) have severe vascular disease or severe osteoporosis.
Your case will be assessed and if we need to seek approval from your medical specialist then we will not start care until you have been given clearance by them.
Yes. Depending on the type of surgery, provided the procedure was not within the previous six months (to allow for complete healing) and there are no surgical implants.
However, this is assessed on a case to case basis
Although this treatment is quite common in the US, UK and parts of Europe it is new to Australia, with a reported success rate of 86%*
However, results can never be promised and you may still require surgery. We will monitor your progress and refer you to your doctor should you/ we not be happy with your progress.
Don’t wait anymore, come visit us at Chiropractic Spinal Decompression clinic and see if Spinal Decompression Therapy is for you!
*Spinal Decompression Research
Surgical Alternatives: Spinal Decompression
CONCLUSION: 86% of the 219 patients who completed the therapy reported immediate resolution of symptoms, while 84% remained pain-free 90 days post-treatment. Physical examination findings showed improvement in 92% of the 219 patients, and remained intact in 89% of these patients 90 days after treatment. It was shown to be effective for herniated and degenerative discs
Journal of Neurologic Research Vol 29, No 3, March 2003
Efficacy of Vertebral Axial Decompression on Chronic Low Back Pain.
CONCLUSION: This 144 patient study showed 76% achieved remission of pain. Except in emergent conditions, Vertebral Axial Decompression should be used on all conditions before surgery is undertaken.
US Musculoskeletal Review 2007
“Magnetic Resonance Imaging Findings After Non-Surgical Spinal Decompression”,
the follow up MRI showed rehydration of the discs at L3/L4, L4/L5, L5/S1 of a herniated disc patient
American Journal of Pain Management Vol 7, No 2, April 1997
Decompression, Reduction, and Stabilization of the Lumbar Spine: A Cost Effective Treatment.
CONCLUSION: Eighty six percent of herniated intervertebral disc patients achieved ‘good’ (50-89% improvement) to ‘excellent’ (90-100% improvement) results with decompression. Sciatica and back pain were relieved. Facet arthrosis patients, 75% obtained ‘good’ to ‘excellent’ results with decompression.
Anesthesiology New Vol 29, no 3 , March 2003
Vertebral Axial Decompression Reduces Chronic Discogenic Low Back Pain-4 Year Study.
CONCLUSION: Four year follow-up after Decompression method shows a sustained 86% reduction in pain and that 91% of patients had resumed their normal activities and has remained pain free
Archives of Physical Medicine and Rehabilitation Medicine Feb 2008
Protocols for Patients with Activity – Limiting Low Back Pain
A total of 296 patients with low back pain and evidence of a degenerative and or herniated disc at 1 or more levels were in this study. 8 Week course of treatment consisting of 5, 30 minute sessions of Decompression Therapy per week for 4 weeks and 1, 30 minute session for a week for 4 additional weeks.
CONCLUSION: Patients showed continued statistical improvement in both pain scores and functional movement scores after their treatment programs were completed for 180 days post-treatment
Evaluating the Effectiveness of Spinal Decompression Therapy
BY BURKHART T, BLUMKE Z, DALEY K, SORENSEN L , HUNT T
Decompression Therapy Evaluationn health information management programs, students participate in real life activities associated with a healthcare organization to apply their acquired knowledge. In this case, the student project included documentation review, data collection, and analysis. Under the supervision of a doctor of chiropractic, the intern was given access to patient records dating from 2011 to 2014.
To track satisfactory rates for the spinal decompression treatment provided in the facility, the electronic health records of 163 randomly chosen patients were examined to record date of treatments, gender, chief complaint, and diagnosis. A section for comments was included from each patient to record medical history, nature of the onset, exacerbating factors, and pain indices throughout the treatment plan. The demographic profile of the patients evaluated was fairly uniform, with a slight majority of women (54 percent) over men (46 percent). The chief complaint listed revealed that over 50 percent of the sample reported some sort of lower back pain. The remainder of complaints comprised such conditions as neck, shoulder, hip, leg, and foot pain.
The clinical evaluation showed a success rate of slightly more than 90 percent, with success defined as patients being “satisfied” or “very satisfied” with the outcome of their treatment. Of the 163 patient charts examined, only 14 patients were classified as “not satisfied” or having deemed the therapy unsuccessful. Four of those patients discontinued their care to seek alternative treatment; namely, a surgical option in an attempt to minimalize pain that was not responding to nonsurgical spinal decompression.
The majority of the patients reported looking forward to receiving care because of the positive results of their treatment, and many were able to avoid surgery. After treatment, patients reported feeling better with minimal pain and overall felt optimistic about receiving chiropractic care. The results of this evaluation exceed the expected outcomes for chiropractic care. Statistical evidence shows that throughout the U.S., more than 75 percent of patients are satisfied with the end result of their chiropractic care (Blumke, 2014). In this evaluation, 91 percent of patients who complained of pain in their back or neck were pleased with their nonsurgical spinal decompression outcome.
Treatment ProtocolsAn effective spinal decompression treatment program consists of five components that lead to positive patient outcomes.
First is a decompression treatment table. There are many on the market but not all are equal in quality.
Second is a pre-decompression treatment protocol such as infrared, laser, heat, or similar therapy to prepare the tissue for the decompressive event. The secret to decompression treatment is that it addresses the biomechanical aspects of disc disease. By creating a phasic physiological change in the spine, the body can repair damaged tissues and the real healing can begin (Aimbire, 2006; Bjordal, 2003; Guehring, 2006).
The third component is nutrition. Look at the patient’s pro-inflammatory diet as a possible cause for their pain and inflammation. This is an often overlooked but critical component. Nutritional recommendations may include dietary change or supplementation, but the chemical mediators that are at work in the patient must be addressed.
The fourth component is posture rehab or exercise therapy. Endurance and stability of the muscle groups supporting the trunk, neck, and head are vital to long-term improvement in spinal function. Many approaches are available including the use of medicine balls, floor exercises, or passive and active physical therapy (Nelson, 1999).
The fifth component of the treatment plan is spinal chiropractic manipulative treatment (CMT). For doctors of chiropractic, CMT is the preferred treatment for patients along with treatment to restore spinal function, reduce pain, and resolve ongoing disability. Recent studies suggest that CMT alone can play a significant role in the regression of disc herniation and resolving radiculopathies associated with degenerative disc disease (Forbush, 2011; Keeney, 2013).
Summary and RecommendationsMORE THAN 31 MILLION AMERICANS EXPERIENCE LOW BACK PAIN at any given time and 80 percent of the population will experience this problem in their lifetime (Forer, 2012). But the surgical option for treating low-back pain often has postoperative complications (Street et al., 2011).
Chiropractic care offers a nonsurgical approach that uses various treatments such as spinal decompression therapy. In a recent study (Gionis and Groteke, 2012), researchers found that 86 percent of patients completing decompression therapy reported resolution of their symptoms. This article details a recent outcome study (Blumke, 2014) completed by a Davenport University health information management intern at a chiropractic center in West Michigan providing spinal decompression treatment. The treatment program described as follows was found to be highly successful with little to no post-treatment complications.
This clinical evaluation of the efficacy of spinal decompression treatment (Blumke, 2014) revealed some notable outcomes and data. An overall successful outcome of 91 percent was seen in cases that had undergone a nonoperative axial spinal decompression treatment plan.
Previous studies have suggested the success rate for spinal decompression treatment to be between 53 and 86 percent (Beattie, 2008; Gose, 1998; Odell, 2003). The practice integrated the five elements of spinal decompression therapy described in this report. These five elements, if applied consistently, can provide patients with successful outcomes. The authors recommend trying them out in your own practice. Begin to integrate pre-decompression therapy with your decompression treatment, add posture rehab, nutritional recommendations, and CMT.
Over the last 10 to 15 years, many doctors of chiropractic have successfully integrated decompression treatment into their practices. Patient outcomes have ranged from poor to great. The doctors who are achieving successful outcomes for their patients, however, have truly “cracked the code” on decompression treatment. They understand that the technology of the table as well as the method in which the care is administered are important. Ultimately, the practitioner must follow a treatment protocol that is safe, cost effective, repeatable, and has measureable results.
The success rate of spinal decompression treatment as noted in this evaluation and the cited studies is especially remarkable when compared to the risk factors for surgical treatment of the same or similar conditions (Street et al., 2012).. Spinal decompression treatment is demonstrably an effective, nonsurgical method for treating patients with neck and lowback pain.
ABOUT THE AUTHORS:
1 TIMOTHY BURKHART, DC, BCIM, partner in Burkhart & Chapp Chiropractic PLC in Grand Rapids, Mich.
2 ZACHARY BLUMKE, Health InformationManagement student, Davenport University in Grand Rapids,Mich.
3 KAREN DALEY, PhD, RN, dean, College of Health Professions, Davenport University in Grand Rapids,Mich.
4 LINDA SORENSEN,MPA, RHIA, CHPS, chair, Health Information Management Department, Davenport University in Grand Rapids,Mich.
5 THOMAS HUNT,MBA, RHIA, CHTS-IM, PhD, associate dean, Health Information Management Department, Davenport University in Grand Rapids,Mich.
REFERENCES:
Aimbire F, et al. Low-level laser therapy iduces dose-dependent reduction of TNFalpha levels in acute inflammation. Photomed Laser Surg. 2006;24(1):33-7.
Beattie PF, Nelson RM, Michener LA, Cammarata J, Donley J. Outcomes after a prone lumbar traction protocol for patients with activity-limiting low back pain: a prospective case series study. Arch Phys Med Rehabil. 2008;89(2):269-74.
Bjordal JM, Couppé C, Chow RT, Tunér J, Ljunggren EA. A systematic review of low level laser therapy with location-specific doses for pain from chronic joint disorders. Aust J Physiother. 2003:49(2):107-16.
Blumke Z. (2014). “How Successful is Chiropractic Care?” Paper submitted to meet the requirements of Davenport University Practicumfor HINT 297C.
Botnick AJ. “Why I Quit Chiropractic.” Chirobase. http://www.chirobase.org/03Edu/botnick.html. Revised August 6, 2013. Accessed Feb 2, 2015.
Forbush SW, Cox T, Wilson E. Treatment of patients with degenerative cervical radiculopathy using a multimodal conservative approach in a geriatric population: a case series. J Orthop Sports Phys Ther. 2011;41(10):723-33.
Forer, B. “Neck Pain: Chiropractors, Exercise Better Than Medication, Study Says.” ABC News. http://abcnews.go.com/blogs/health/2012/01/04/neck-pain-chiropractors-exercisebetter-than-medication-study-says. Published January 4, 2012. Accessed February 2, 2015.
Gionis TA, Groteke E. (2012). “Spinal decompression: The outcome of a clinical study.” [Blog post]. Pro-Care Medical Center. http://www.procaremedcenter.com/surgicalalternatives-spinal-decompression. Published May 18, 2010. Accessed Feb 2, 2015.
Gose EE, Naguszewski WK, Naguszewski RK. Vertebral axial decompression therapy for pain associated with herniated or degenerated discs or facet syndrome: an outcome study. Neurol Res. 1998;20(3):186-90.
Guehring T, et al. Disc distraction shows evidence of regenerative potential in degenerated intervertebral discs as evaluated by protein expression, magnetic resonance imaging, and messenger ribonucleic acid expression analysis. Spine (Phila Pa 1976). 2006;31(15):1658-665.
Hall H. “Top 10 Chiropractic Studies of 2013.” Science-Based Medicine. http://www.sciencebasedmedicine.org/top-10-chiropractic-studiesof-2013. Published January 21, 2014. Accessed February 2, 2015.
Centers for Medicare and Medicaid Services. “Article for Chiropractic Services – Supplemental Instructions Article (A47385).” CMS.gov. http://apps.ngsmedicare.com/SIA/ARTICLE_A47385.htm. Published November 1, 2008. Updated April 1, 2010. Accessed Feb 2, 2015.
Keeney BJ, et al. Early predictors of lumbar spine surgery after occupational back injury: results from a prospective study of workers in Washington State. Spine (Phila Pa 1976). 2013;38(11):953-64.
Nelson BW, et al. Can spinal surgery be prevented by aggressive strengthening exercises? A prospective study of cervical and lumbar patients. Arch Phys Med Rehabil. 1999;80(1):20-25.
Odell R, et al. Decompression Reduces Chronic Back Pain: 4 Year Study. Anesthesiology News. 2003;29(3):14-15.
Street JT, et al. Morbidity and mortality of major adult spinal surgery. A prospective cohort analysis of 942 consecutive patients. Spine J.2012;12(1):22-34.
 0416 020 512
0416 020 512

